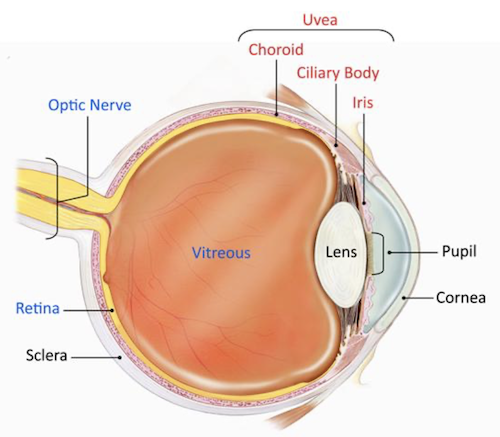
A rare disease, uveitis is an inflammatory condition affecting the “uvea” or middle layer of the eye. However, the term is commonly used to refer to any inflammation of the eye. Uveitis can occur at any age and affect one or both eyes. Early diagnosis and appropriate treatment are critical to preserving vision and preventing complications.
Types of Uveitis
Uveitis is classified by the location, and there are several different types:
- Scleritis – affects the sclera, or the “white” part of the eye
- Iritis/Iridocyclitis – affects the iris and ciliary body in the front of the eye
- Pars planitis/intermediate uveitis – affects the middle part of the eye, including the vitreous and retina
- Posterior uveitis – affects the retina and choroid in the back of the eye
- Panuveitis – affects the entire uvea
Diagnosing Uveitis
At your appointment, we will discuss your medical and family history to help identify any potential underlying causes of your inflammation. If you have a systemic autoimmune or inflammatory disease like rheumatoid arthritis, lupus or inflammatory bowel disease (IBS), it can increase your risk of developing uveitis. Additional risk factors include infections like shingles, herpes, Lyme disease or syphilis as well as parasites such as toxoplasmosis.
We will also perform a comprehensive, dilated eye exam along with a tonometry test to check your eye pressure. Depending on your condition, we may also have you complete an optical coherence tomography (OCT) or fluorescein angiography test. Finally, if we suspect a systemic or infectious cause of your uveitis, we will order blood tests and possible, additional imaging studies.
Treating Uveitis
Uveitis treatment aims to control inflammation, relieve pain, preserve vision and prevent recurrence. Each patient’s treatment must be customized to control the level of inflammation and reduce possible side effects.
Treatments can include:
- Corticosteroid eye drop medications that reduce inflammation
- Dilating eye drops to help reduce pain and swelling
- Intravitreal injections or implants of steroid medication
- Oral medication
- Biologic therapies like infliximab or adalimumab, tumor necrosis factor-alpha (TNF-α) inhibitors, which may be used for non-infectious uveitis that is unresponsive to corticosteroids
Too often, steroids are overused to treat uveitis, which can cause local side effects like cataracts and glaucoma along with systemic side effects, including weight gain, diabetes, hypertension and osteoporosis. That is why it is important to seek care from a fellowship-trained uveitis specialist who uses steroid sparing therapy to save sight.
Additionally, some patients will need regular blood tests to ensure that their treatment medication is not causing problems. Finally, some forms of uveitis are chronic and will need to be treated for a long time, often years.
Texas Retina has two fellowship-trained physicians who sub-specialize in treating uveitis: Robert C. Wang, MD, and Rene Y. Choi, MD.
Click HERE to learn more about uveitis care at Texas Retina.