Age-related macular degeneration (AMD) is the leading cause of vision loss in older American adults and the most common reason patients are referred to Texas Retina Associates. It happens when a part of the retina called the macula is damaged. The macula is the central part of the retina responsible for detailed vision tasks.
Loading...
Dry AMD
This is the most common form. In fact, about 80% of people who have AMD have the dry form. Dry AMD is characterized by accumulation of yellow deposits called drusen, thinning of the macula, and gradual deterioration of central vision.
Geographic atrophy (GA), a late stage of dry AMD, involves chronic and irreversible progressive destruction (atrophy) of central retinal cells and underlying blood vessels due to chronic inflammation. Upon examination by an ophthalmologist or retina specialist, these areas of atrophy often look like a map which led to the term “geographic atrophy.” GA gradually causes permanent loss of visual acuity. It can occur in one eye or both, but if a patient has it in one eye, they are more likely to develop it in the other as well. The condition may remain asymmetric (unequal) in the other eye for a while and progresses slowly.
Wet AMD
While much less common, wet AMD is more serious. With wet AMD, abnormal blood vessels grow under the retina and may leak, causing accumulation of blood or other fluid. This can cause scarring of the macula. In contrast with dry AMD, patients with wet AMD often, but not always, experience sudden and severe visual loss.
Symptoms
Patients with AMD may notice a worsening of their central vision while retaining good peripheral vision. Symptoms include, but are not limited to:
- Blurred central vision
- Increasing difficulty with reading
- Patchy visual loss
- Distortion or warping of straight objects
However, even patients with advanced macular disease tend to retain excellent peripheral vision.
Risk Factors
Macular degeneration primarily affects older, white individuals. However, cases have been reported in younger patients and those not of Caucasian descent. Additional risk factors predispose people to the development and progression of the disease, including:
- Poor diet (high in saturated fat) and being overweight
- High cholesterol
- Cardiovascular disease
- Cigarette smoking
- Sunlight exposure
- Having a family member with AMD
Much research has been done regarding the genetics of AMD. Adult relatives of AMD patients should schedule an appointment with a retina specialist and undergo a baseline evaluation and dilated eye exam.
Diagnosis
Dry and wet macular degeneration impact vision in different ways and are also treated quite differently. Our physicians will use a variety of clinical tests and exam techniques to better characterize your individual situation, make an accurate diagnosis, and optimize treatment.
During an initial visit for macular degeneration, patients typically undergo two tests:
Fluorescein Angiography (FA)
FA is considered the “gold standard” for differentiating between dry and wet AMD. It involves the injection of a small amount of a yellow, vegetable-based dye through a patient’s peripheral vein – usually the arm or hand. Shortly after, a certified ophthalmic angiographer will take a series of time-dependent retinal photographs. The injected dye lights up the retina’s intricate vascular network. This helps our specialists pinpoint areas of leakage in those patients with wet macular degeneration and target specific zones with specialized laser therapy when needed.
Optical Coherence Tomography (OCT)
OCT is a non-invasive, quick exam that is used to visualize the retinal microarchitecture. A machine scans the retina and provides very detailed images of the retina and macula. Sometimes it will uncover tiny areas of fluid or retinal irregularity not readily apparent to a retina specialist during a microscopic exam.
Patients play an important role in diagnosis and care of AMD: The Amsler Grid
Despite recent advances in ophthalmic imaging, there is no single test that can be relied upon to direct treatment and clinical decision-making. A patient’s relationship with his or her Texas Retina specialist is at the core of our practice philosophy, and good patient-physician communication is critical. Important decisions about retinal health are very much a joint effort. The patient’s perception of his or her visual health and the patient’s perception of any vision changes, however slight, is every bit as important in directing care as are the clinical tests.
As a result, every patient diagnosed with macular degeneration should establish a daily routine for monitoring their own vision. This is most simply and reliably performed with an Amsler grid, a simple graph paper-like patchwork of straight vertical and horizontal lines, which we are happy to provide at no cost – simply ask one of our nurses.
Often, patients with subtle progression of macular disease will report new “waviness” or “missing areas” when monitoring their grid. Should you or a family member notice new changes on an Amsler grid, contact us promptly. One of our retina specialists or trained ophthalmic nurses is always available to consult with you by phone. As a general rule, patients who receive treatment in timelier fashion tend to fare better than those who delay evaluation by a retina specialist.
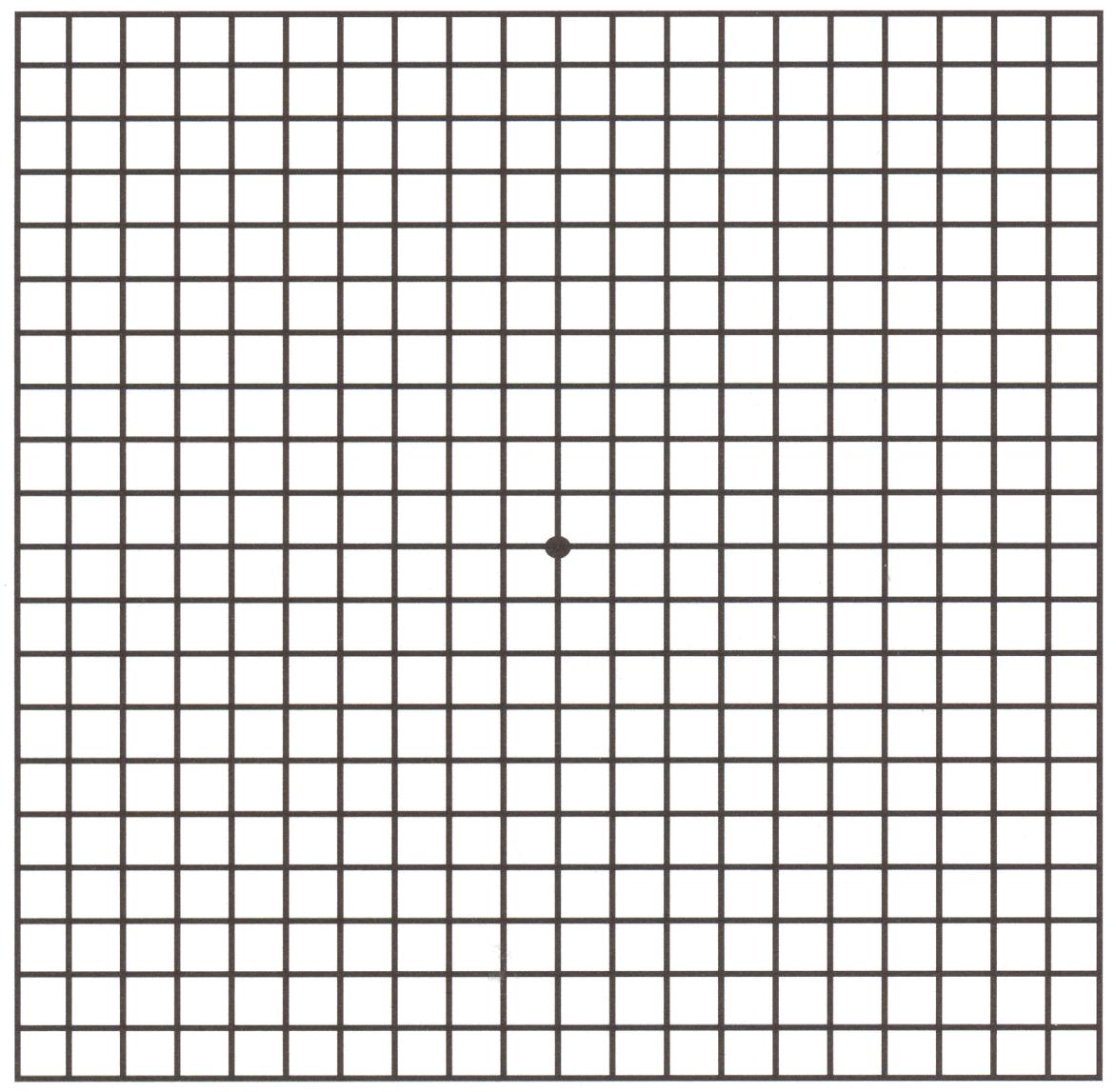
Amsler Grid
Treatment
Medical researchers have thrown themselves fully into the battle against macular degeneration, and dramatic progress has been made in the effort to combat age-related vision loss. At Texas Retina, many of our physicians have helped lead this ground-breaking research to bring the latest treatment options to our patients here in Texas.
Wet AMD
The most effective treatments for wet AMD are medications that block a molecule called VEGF (Vascular Endothelial Growth Factor). VEGF causes growth of “leaky” blood vessels in wet macular degeneration. These anti-VEGF medications include Avastin, Lucentis, and Eylea, and they help to reduce the number of abnormal blood vessels in your retina. All of these medications are introduced directly into the eye through a tiny needle. While the thought of an “eye shot” might cause many to cringe, in our experience, there is little, if any, patient discomfort, and the spectacular visual gains far outweigh any fears.
In contrast to prior treatments, anti-VEGF medications have actually improved vision for many patients with wet macular degeneration. Several large national and international studies have shown that Avastin, Lucentis, and Eylea all work well. Your retina specialist will discuss with you which medication may be best suited for your situation.
Laser surgery may also be used to treat some types of wet AMD. Your eye surgeon shines a laser light beam on the abnormal blood vessels. This reduces the number of vessels and slows their leaking.
In general, repeated injections are the norm in order to keep the fluid from recurring. Researchers continue to explore new medications that may restore vision even better and prolong the interval between injections. Texas Retina is involved in several clinical trials to explore new treatment options. Should you have an interest in participating in a trial, please inform your retina specialist during your next visit.
Dry AMD
For many years, there was no way to treat the dry form of AMD other than vitamin supplements that the Age-Related Eye Disease Study (AREDS) demonstrated could slow progression. However, on February 17, 2023, the U.S. Food and Drug Administration (FDA) approved intravitreal pegcetacoplan (brand name Syfovre), the first-ever treatment for GA secondary to AMD. Texas Retina Associates was involved in the Phase III clinical trial (OAKS) that led to the approval and is also part of the extension study (GALE) that will evaluate the long-term impact of this treatment.
In addition, Texas Retina Associates has been involved in several other Phase II and III clinical trials to test additional potential new treatment options for GA. This includes the Phase III GATHER1 and GATHER2 trials of another drug called avacincaptad pegol (Zimura) as well as the SIGLEC trial of AVD-104, a novel glycan-coated intravitreal nanoparticle designed to alleviate chronic, non-resolving inflammation that can occur with GA. Once again, please let your Texas Retina physician know if you are interested in participating in one of our current clinical trials.

